 Visto che la lista è troppo lunga per commentare ogni citazione, ho controllato solo il primo tema, cioè quello che riguarda l'asma e le allergie. Prima di tutto ho cercato di tutti i 14 lavori qui elencati l'abstract e dove era possibile anche il testo integrale. Commenterò uno per uno. Visto che la lista è troppo lunga per commentare ogni citazione, ho controllato solo il primo tema, cioè quello che riguarda l'asma e le allergie. Prima di tutto ho cercato di tutti i 14 lavori qui elencati l'abstract e dove era possibile anche il testo integrale. Commenterò uno per uno.
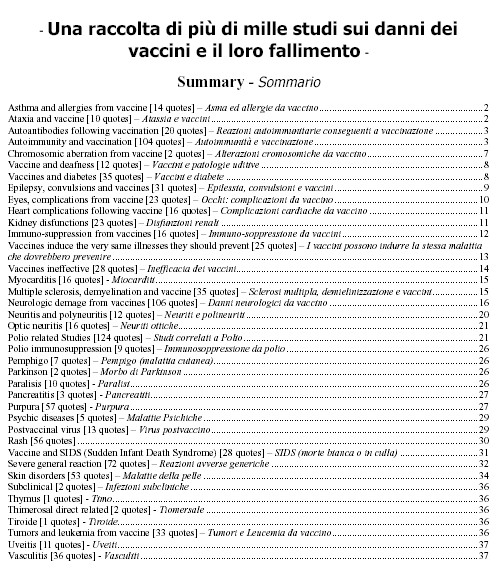
Asthma and allergies from vaccine [14 quotes] - Asma ed allergie da vaccino
1) "Is infant immunization a risk factor for childhood asthma or allergy?",
Epidemiology 1997 Nov;8(6):678-80 Kemp T; Pearce N; Fitzharris P; Crane J; Fergusson D; St. George I; Wickens K; Beasley R;
Department of Medicine, Wellington School of Medicine, New Zealand.
The Christchurch Health and Development Study comprises 1,265 children born in 1977. The 23 children who received no diphtheria/pertussis/tetanus (DPT) and polio immunizations had no recorded asthma episodes or consultations for asthma or other allergic illness before age 10 years; in the immunized children, 23.1% had asthma episodes, 22.5% asthma consultations, and 30.0% consultations for other allergic illness. Similar differences were observed at ages 5 and 16 years. These findings do not appear to be due to differential use of health services (although this possibility cannot be excluded) or con-founding by ethnicity, socioeconomic status, parental atopy, or parental smoking.
il mio commento:
Questo studio non è di buona qualità e non permette di raggiungere a
conclusioni valide. Il numero di bambini NON vaccinati (23 su un totale di
1.265) è troppo piccolo per fare un confronto. Quindi: NON SIGNIFICATIVO
2) Alm JS; Swartz J; Lilja G; Scheynius A; Pershagen G Johan.Alm@sos.ki.se ; Atopy in children of families with an anthroposophic lifestyle [see comments]; Lancet 1999 May 1;353(9163):1485-8
Lancet. 1999 May 1;353(9163):1485-8.
Atopy in children of families with an anthroposophic lifestyle.
Alm JS, Swartz J, Lilja G, Scheynius A, Pershagen G.
Department of Laboratory Medicine, Karolinska Institute and Hospital,
Stockholm, Sweden. Johan.Alm@sos.ki.se
BACKGROUND: Increased prevalence of atopic disorders in children may be associated with changes in types of childhood infections, vaccination
programmes, and intestinal microflora. People who follow an anthroposophic way of life use antibiotics restrictively, have few vaccinations, and their diet usually contains live lactobacilli, which may affect the intestinal microflora. We aimed to study the prevalence of atopy in children from anthroposophic families and the influence of an anthroposophic lifestyle on atopy prevalence. METHODS: In a cross-sectional study, 295 children aged 5-13 years at two anthroposophic (Steiner) schools near Stockholm, Sweden, were compared with 380 children of the same age at two neighbouring schools in terms of history of atopic and infectious diseases, use of antibiotics and vaccinations, and social and environmental variables. Skin-prick tests were done for 13 common allergens, and we took blood samples from children and their parents for analysis of allergen-specific serum IgE-antibodies.
FINDINGS: At the Steiner schools, 52% of the children had had antibiotics in the past, compared with 90% in the control schools. 18% and 93% of children, respectively, had had combined immunisation against measles, mumps, and rubella, and 61% of the children at the Steiner schools had had measles. Fermented vegetables, containing live lactobacilli, were consumed by 63% of the children at Steiner schools, compared with 4.5% at the control schools.
Skin-prick tests and blood tests showed that the children from Steiner
schools had lower prevalence of atopy than controls (odds ratio 0.62 [95% CI 0.43-0.91]). There was an inverse relation between the number of
characteristic features of an anthroposophic lifestyle and risk of atopy (p
for trend=0.01).
INTERPRETATION: Prevalence of atopy is lower in children from anthroposophic families than in children from other families. Lifestyle factors associated with anthroposophy may lessen the risk of atopy in childhood.
il mio commento:
Anche questo studio è di pessima qualità e non serve a nulla - perché non si può osservare "uno stile di vita", buttando dentro tanti parametri,
mescolare bene, e poi interpretare il risultato a piacere. Uno può pescare
dal sacco dei parametri "allattamento al seno" e dire: Questo studio
dimostra che l'allattamento protegge dall'asma. Poi viene un'altro e pesca
dal sacco "vaccinazioni in generale" e dice: "Questo studio dimostra che il
non-vaccinare protegge i bambini dall'asma". Un terzo pesca dal sacco "il
sapone fatto in casa" o "il cibo biologico" o "l'imbottitura del letto" e
così fino all'inifinito. Questo è un'ottimo esempi di uno studio pieno di
confounding-bias = elementi di disturbo. La statistica è una cosa complicata ed è fin troppo facile che studi fatti coi piedi come questo vengano poi sfruttati da gente che vuole dimostrare qualcosa. Anch'io Vi ho dimostrato qualcosa con questo "studio".
Quindi il numero due: NON SIGNIFICATIVO
3) Casale TB, Bernstein IL, Busse WW, LaForce CF, Tinkelman DG, Stoltz RR, Dockhorn RJ, Reimann J, Su JQ, Fick RB Jr, Adelman DC., "Use of an anti-IgE humanized monoclonal antibody in ragweed-induced allergic rhinitis", J Allergy Clin Immunol 1997 Jul;100(1):110-21
Department of Internal Medicine, University of Iowa, Iowa City, USA.
BACKGROUND: Increased serum levels of antigen-specific IgE are often
associated with allergic respiratory disorders. RhuMAb-E25, a recombinant
humanized monoclonal antibody, decreases free serum IgE by forming
biologically inactive immune complexes with free IgE.
OBJECTIVE: We hypothesized that rhuMAb-E25 would decrease total serum IgE and reduce
symptoms.
METHODS: Two hundred forty subjects were enrolled into five groups to determine the safety, tolerance, and efficacy of repeated administration of rhuMAb-E25 in adults with ragweed-induced allergic rhinitis and to explore the pharmacodynamic relationship of rhuMAb-E25 and IgE. One hundred eighty-one subjects received an initial intravenous loading dose (day 0, 1 month before ragweed season), followed by administration of rhuMAb-E25 (in mg/kg body weight) of 0.15 mg/kg subcutaneously, 0.15 mg/kg intravenously, or 0.5 mg/kg intravenously on days 7, 14, 28, 42, 56, 70, and 84. A subcutaneous placebo group and an intravenous placebo group were included. The total evaluation time included the 84-day treatment period, followed by a 42-day observation period.
RESULTS: Adverse events were mild, and no differences were observed in the rates between the three active and two placebo treatment groups. Ragweed-specific IgE levels correlated with symptom scores. RhuMAb-E25 decreased serum free IgE levels in a dose- and baseline IgE-dependent fashion. However, only 11 subjects had IgE levels
that were suppressed to undetectable levels (< or = 24 ng/ml), a sample too small to demonstrate significant differences and clinical efficacy. Thus the case for efficacy was not proven. Nonetheless, the study confirms that it is safe to repeatedly administer rhuMAb-E25 over a period of months.
CONCLUSIONS: Because rhuMAb-E25 decreased serum free IgE in a dose-dependent fashion and because symptom scores correlated with antigen-specific IgE levels, the results suggest that if given in adequate doses, rhuMAb-E25 should be an effective therapy for allergic diseases.
il mio commento:
Che cosa c'entra una sperimentazione con un farmaco per la cura della febbre da fieno con l'asma, le allergie e i vaccini? Assolutamente niente.
Ergo: NON PERTINENTE
4) Ekbom K., "A case of asthma after vaccination against smallpox", Acta Med
Scand Suppl. 1966;464:170-1.
Acta Med Scand Suppl. 1966;464:170-1.
A case of asthma after vaccination against smallpox.
il mio commento:
E' la descrizione di UN caso di asthma del 1966 DOPO la vaccinazione contro il vaiolo (non vuol dire che è stata causata dal vaccino).Che cosa ci interessa il vaccino contro il vaiolo? Questo vaccino non è più in uso da decenni perché la malattia, grazie alle vaccinazioni di massa in tutto il mondo, è stata debellata (durante le frequenti epidemie aveva ucciso il 15-20% delle persone che si ammalavano di vaiolo).
Quindi: NON PERTINENTE
5) Goldman II., [Allergic rhinosinusbronchopathy in a patient after the use
of dry anti-influenza serum],Vestn Otorinolaringol. 1966 Mar-Apr;28(2):98-9.
il mio commento:
Un'altra descrizione (in lingua russa) di una caso, questa volta dopo un serum anti-influenza (che non è un vaccino) del 1966. Chissà che cosa è una Allergic rhinosinusbronchopathy
Quindi: NON PERTINENTE
6) Hurwitz EL, Morgenstern H., "Effects of diphtheria-tetanus-pertussis or
tetanus vaccination on allergies and allergy-related respiratory symptoms
among children and adolescents in the United States", J Manipulative Physiol Ther 2000 Feb;23(2):81-90
J Manipulative Physiol Ther. 2000 Feb;23(2):81-90.
Effects of diphtheria-tetanus-pertussis or tetanus vaccination on allergies
and allergy-related respiratory symptoms among children and adolescents in the United States.
Hurwitz EL, Morgenstern H. UCLA School of Public Health, Department of Epidemiology, Los Angeles, Calif 90095-1772, USA.
BACKGROUND: Findings from animal and human studies confirm that diphtheria and tetanus toxoids and pertussis (DTP) and tetanus vaccinations induce allergic responses; associations between childhood vaccinations and subsequent allergies have been reported recently. OBJECTIVE: The association of DTP or tetanus vaccination with allergies and allergy-related respiratory symptoms among children and adolescents in the United States was assessed.
METHODS: Data were used from the Third National Health and Nutrition
Examination Survey on infants aged 2 months through adolescents aged 16 years. DTP or tetanus vaccination, lifetime allergy history, and allergy
symptoms in the past 12 months were based on parental or guardian recall. Logistic regression modeling was performed to estimate the effects of DTP or tetanus vaccination on each allergy.
RESULTS: The odds of having a history of asthma was twice as great among vaccinated subjects than among unvaccinated subjects (adjusted odds ratio, 2.00; 95% confidence interval, 0.59 to 6.74). The odds of having had any allergy-related respiratory symptom in the past 12 months was 63% greater among vaccinated subjects than unvaccinated subjects (adjusted odds ratio, 1.63; 95% confidence interval, 1.05 to 2.54). The associations between vaccination and subsequent allergies and symptoms were greatest among children aged 5 through 10 years.
CONCLUSIONS: DTP or tetanus vaccination appears to increase the risk of
allergies and related respiratory symptoms in children and adolescents.
Although it is unlikely that these results are entirely because of any
sources of bias, the small number of unvaccinated subjects and the study
design limit our ability to make firm causal inferences about the true
magnitude of effect.
il mio commento: Questo studio ha lo stesso difetto del lavoro di Kemp (il primo nella presente lista). Solo l'1% dei soggetti NON è vaccinato. Quindi non è possibile fare un valido confronto.
Quindi: NON SIGNIFICATIVO
Per chi sa l'inglese consiglio di leggere il commento su questo
studio, che include anche i commenti di quelli che Hurwitz cita (fra cui
alcuni di questa lista che ci ha mandato Gil). E' molto interessante
![http://www.geocities.com/issues_in_immunization/safety/Hurwitz_review.htm]()
7) Lewis SA, Britton JR, "Measles infection, measles vaccination and the
effect of birth order in the aetiology of hay fever", Clin Exp Allergy 1998
Dec;28(12):1493-500
Clin Exp Allergy. 1998 Dec;28(12):1493-500.
Measles infection, measles vaccination and the effect of birth order in the
aetiology of hay fever.
Lewis SA, Britton JR.
Division of Respiratory Medicine, University of Nottingham, City Hospital,
UK.
BACKGROUND: It has recently been suggested that measles infection may reduce the risk of atopy. OBJECTIVE: To study the independent effect of measles infection and measles vaccination on the occurrence of hay fever in a British national birth cohort.
METHODS: In over 6000 children born in 1970, details of immunizations and childhood diseases were collected by parental interviews at ages 5, 10 and 16 years, and hay fever within the past year at age 16 years. RESULTS: In univariate analysis, hay fever was less common in those contracting measles infection than in those not infected (OR 0.86, 95% CI 0.76-0.96), and more common in those given measles vaccination than in those not vaccinated (OR 1.16, 95% Cl 1.03-1.31). However, these effects were strongly confounded by birth order, which was closely associated with the likelihood of receiving measles vaccination and with the risk of hay fever. A strong interaction between the effects of measles vaccination and infection, and birth order was found, such that in those with many older sibling contacts, hay fever was significantly and independently reduced in relation to both measles infection and measles vaccination relative to those who were neither infected nor vaccinated.
CONCLUSIONS: Both measles infection and measles vaccination in childhood appear to reduce the risk of hay fever in children with multiple older sibling contacts. Differential exposure or response to the measles virus may explain the effect of birth
order on the occurrence of allergic disease.
il mio commento:
Gli autori dello studio concludono: "Sia il morbillo che il vaccino contro il morbillo durante l'infanzia, sembrano ridurre il rischio di febbre da fieno in bambini con
molti fratelli più grandi." Questo studio non sostiene per niente la tesi
che "le vaccinazioni causano l'asma e le allergie". Risulta invece che l'ordine di nascita e del numero di fratelli più grandi influiscono alla comparsa di allergie al
polline.
Quindi: NON PERTINENTE
Cool McIntyre PB, O'Brien ED, Heath TC., "Immunisation and asthma", Commun Dis Intell. 1998 Mar 19;22(3):38.
Commun Dis Intell. 1998 Mar 19;22(3):38.
Immunisation and asthma.
McIntyre PB, O'Brien ED, Heath TC.
National Centre for Immunisation Research and Surveillance of Vaccine
Preventable Diseases (NCIRS), Royal Alexandra Hospital, New South Wales.
il mio commento:
In questa pubblicazione McIntyre porta le prove che il vaccino MPR non causa allergie. Che questo viene inserito in una lista come la presente è proprio il colmo.
Quindi: PROVA IL CONTRARIO
9) Muhlemann K; Alexander ER; Weiss NS; Pepe M; Schopfer K, "Risk factors for invasive Haemophilus influenzae disease among children 2-16 years of age in the vaccine era, Switzerland 1991-1993. The Swiss H. Influenzae Study Group", Int J Epidemiol 1996 Dec;25(6):1280-5
Institute of Medical Microbiology, University of Berne, Switzerland.
BACKGROUND: Continued surveillance, and detailed investigation of direct and indirect effects of conjugated vaccines and risk factors for invasive
H.influenzae serotype B (Hib) disease in the vaccine era are important.
METHODS: 143 cases with invasive disease between 1991 and 1993 aged 2-16 years were selected retrospectively from a large incidence trend study. Controls (n = 336) were recruited from local vital registries and matched to cases for age, gender, and residence. Hib vaccination histories among study subjects and their siblings and other sociodemographic variables were obtained by questionnaires completed by the parents of these children. Adjusted odds ratio (OR) estimates were calculated by conditional logistic regression analysis.
RESULTS: Most vaccinated subjects had received the Polysaccharide-Diphtheria Toxoid vaccine and estimated vaccine efficacy was high (95%; 95% confidence interval [CI] 60-99%). Also, the results suggested that protection afforded by vaccination against Hib extended to the family members of vaccinated children. School attendance was found to be protective against invasive Hib disease (OR:0.33; CI:1.2-14.4). Cases more often than controls reported suffering from asthma and allergies (OR:4.8; CI:1.2-19.4).
CONCLUSIONS: Post-licensure vaccine efficacy is high among children > or = 2 years of age. The observed association between asthma and epiglottitis is novel and deserves further investigation.
il mio commento:
Questo lavoro controlla l'efficacia del vaccino contro HIB (che può causare
la meningite e la epiglottite - quest'ultima può portare alla morte per
soffocamento entro pochi minuti). Il risultato è che il vaccino usato
(Polysaccharide-Diphtheria Toxoid) ha un'alta efficiacia = 95%. Si è anche
visto che fra i bambini che si sono ammalati di HIB c'è stata una maggiore
incidenza di asma e di allergie.
Quindi: IMPERTINENTE e anche a favore della vaccinazione contro HIB per
quanto riguarda l'incidenza asma e allergie.
10) Odent, MR et al; Pertussis Vaccination and Asthma : is there a link ? ;
JAMA 1994- Vol. 272, No. 8 pag. 592-593
il mio commento: Non si tratta di uno studio, ma di una lettera che Odent ha mandato a Jama in cui riporta un sondaggio (non controllato) per niente scientifico fatto da lui.
Quindi: NON SIGNIFICATIVO
11) Reed CE., "Pertussis sensitization as an animal model for the abnormal bronchial sensitivity of asthma", Yale J Biol Med. 1968 Apr-Jun;40(5):507-21.
Yale J Biol Med. 1968 Apr-Jun;40(5):507-21.
il mio commento: Anche di questo non ho trovato abstract. Dal titolo sembra che l'autore parlasse di "pertosse" e non di un vaccino antipertosse. Per di più si tratta di uno studio su animali.
Quindi: NON PERTINENTE
12) Reizis Z, Frank J, Sikuler E., [Allergic vasculitis and bronchial asthma following influenza vaccination], Harefuah. 1987 Jan 15;112(2):70-1.
13) Singh M., "Influenza vaccination and asthma", Indian Pediatr. 2000
Apr;37(4):459-60.
Indian Pediatr. 2000 Apr;37(4):459-60.
Advanced Pediatric Center, Post Graduate Institute of Medical Education and Research, Chandigarh 160 012, India.
Exacerbations in children with asthma are often associated with viral
infections(1). Although the contribution by influenza virus to this
exacerbation has not been fully quantified several guidelines recommend
immunization of asthmatic subjects against influenza. A question is asked in various forums whether there should be a policy to vaccinate children with influenza vaccine in India. The primary goal of influenza vaccination policy has been the reduction of excess deaths associated with influenza epidemics(2). While influenza may cause asthma exacerbations, there has been concern that vacciantion may precipitate an asthma attack in some people. One previously done review had concluded that this vaccine does not benefit patients of asthma an chronic obstructive pulmonary disease(3). A recent Cochrane review has addressed this problem systematically to assess the effects of influenza vaccination in children and adults with asthma(4). The source of the articles included in the review was the Cochrane Airways Groups trials register which is a data base maintained by the Cochrane airways group with its editorial base at London. The reference lists of articles were also checked.
Randomized trials of influenza vaccination in children (over two years of
age) and adults with asthma were included. People with chronic obstructive
pulmonary disease were excluded. Inclusion criteria and assessment of trial quality were applied by two reviewers independently. Data extraction was done by two reviewers independently. Study authors were contacted for missing information.
Nine trials were analyzed. Four of these trials were of high quality. The
studies covered a wide diversity of people, settings and types of influenza
vaccination, so data from the different trials were not pooled. In one
trial, no protective effect of influenza vaccination against asthma
exacerbation was demonstrated, but the incidence of influenza was low
during the study period. A higher number of asthma exacerbations following killed influenza vaccination was found in one trial (risk difference 3.1%, 95% confidence interval 0.3% to 5.9%). When people with upper respiratory tract infections were excluded, this difference was no longer significant. A small trial using recombinant vaccine found no significant difference in asthma exacerbations between the vaccinated and placebo groups.
The reviewers did not find enough evidence to assess the benefits and risks of influenza vaccination for people with asthma. Whatever evidence is
available is not of sufficient quality to assess the usefulness of this
vaccine in asthmatic subjects. It has been recommended that large randomized controlled trials be conducted with sufficient power to detect the difference in the exacerbation rate amongst these individuals. Moreover, in countries like India where enough information is not available about the prevailing influenza virus strains this vaccine which has a potential to be ineffective after a few years even in the countries where it is produced cannot be routinely recommended.
Meenu Singh,
Associate Professor,
Advanced Pediatric Center,
Post Graduate Institute
of Medical Education and Research,
Chandigarh 160012, India.
References
1. McIntosh K, Ellis EF, Hoffman LS, Lyban TG, Ellis JJ, Fulginiti VA. The
association of viral and bacterial respiratory infections with exacerbation
of wheezing in young asthmatics. J Pediatr 1973; 82: 578-590.
2. Barker WH, Mulloly JP. Pneumonia and influenza deaths during epidemics.
Arch Int med 1982; 142: 85-89.
3. Rothbath PH, Kemper BM, Sprenger MJ. Sense and nonsense of influenza
vaccination in asthma and chronic obstructive pulmonary disease. Am J Respir
Crit Care Med 1995; 151: 1682-1686.
4. Cates CJ, Jefferson TO, Bara AL. Vaccines for preventing influenza in
people with asthma. The Cochrane Library, 1999, Issue 4. Update Software.
Oxford, UK.
il mio commento:
Questo è la lettera di un medico indiano (dell'India) che riporta un review
di alcuni studi. Lui cerca di trovare evidenza negli studi fatti fino a quel
momento (2000), se il vaccino anti-influenzale sia indicato per persone che Soffrono di asma oppure no. Gli studi che lui menziona hanno controllato se le persone vaccinate contro l'influenza, sono più protette da un peggioramento di asma di quelli che non sono stati vaccinati. Ebbene: la conclusione è che (al 2000) lui non ha trovato né prove sufficienti a favore della raccomandazione di fare questo vaccino alle persone con l'asma, né prove sufficienti per il contrario.
Ergo: NON PERTINENTE!
14) Watson JM, Cordier JF, Nicholson KG., "Does influenza immunisation cause exacerbations of chronic airflow obstruction or asthma?", Thorax. 1997 Feb;52(2):190-4.
Thorax. 1997 Feb;52(2):190-4.
Watson JM, Cordier JF, Nicholson KG.
PHLS Communicable Disease Surveillance Centre, London, UK.
il mio commento:
Il lavoro originale si trova qui:
http://thorax.bmjjournals.com/cgi/reprint/52/2/190.pdf. Nemmeno questo, l'ultimo dell'elenco vale per sostenere la loro tesi che i vaccini causano l'asma.
In questo lavoro sono stati rivisti tutti gli studi sul tema "aumenta il
vaccino anti-influenzale l'aggravamento acuto dell'ostruzione delle vie
respiratorie o l'asma?" e non si è trovato nessuno studio che provasse che
lo faccia. Dice che gli studi finora fatti sono piccoli e che ci vorrebbero
studi con più soggetti per poter definitivamente escludere che il vaccino
possa peggiorare queste situazioni respiratorie.
Quindi: NON PERTINENTE
Sono giunta alla fine di questo lavoro. E' stato istruttivo?
Conclusione: Nessuno dei 14 studi citati provava un nesso causale tra qualsiasi vaccino e asma o allergie.
|



 Visto che la lista è troppo lunga per commentare ogni citazione, ho controllato solo il primo tema, cioè quello che riguarda l'asma e le allergie. Prima di tutto ho cercato di tutti i 14 lavori qui elencati l'abstract e dove era possibile anche il testo integrale. Commenterò uno per uno.
Visto che la lista è troppo lunga per commentare ogni citazione, ho controllato solo il primo tema, cioè quello che riguarda l'asma e le allergie. Prima di tutto ho cercato di tutti i 14 lavori qui elencati l'abstract e dove era possibile anche il testo integrale. Commenterò uno per uno.